Exploring SART
Answering the Top Six Questions about IVF with Data and Tools from the Society of Assisted Reproduction

In medical terms, in-vitro fertilization (IVF) is an elective procedure.
I know. You’re probably thinking, “Excuse me? There is nothing elective about this experience.”
True.
But, in medicine, the term “elective” doesn’t necessarily mean optional. It just means that the procedure isn’t needed to address an immediate threat - it can be planned for and scheduled in advance.
Examples of other elective procedures include knee and hip replacements, surgeries to fix hernias and mastectomies to treat breast cancer.
Because elective procedures can be planned for, patients have the opportunity to research and prepare for them.
Typically, whether considering IVF or a knee replacement, there are six things that patients want to know:
1. What is it?
2. Does it work?
3. Will it work for me?
4. What are the risks?
5. What does it cost?
6. Who is the best doctor for me?

1. What is it?
2. Does it work?
3. Will it work for me?
4. What are the risks?
5. What does it cost?
6. Who is the best doctor for me?

Although these questions seem straightforward, it is surprising how hard it can be to find the information we need to answer them.
Thankfully, in the case of IVF, the Society for Assisted Reproductive Technology (SART) has been publishing information and data about IVF since 1995.
SART is the primary organization of professionals in the United States dedicated to the practice of assisted reproductive technologies (ART).
Its mission is to establish and maintain ART standards so that patients receive the best possible care. It does this by:
- publicly reporting the IVF birth outcomes of its member clinics.
- setting guidelines for best practices in ART and requiring all member clinics to adhere to them.
- participating in patient advocacy and regulatory review.
- offering consultative services to clinics trying to improve their practices and outcomes.
Roughly 86% of US IVF clinics are SART members and report their IVF outcomes to the organization. Therefore, it holds one of the largest databases of IVF outcomes in the country.
In this article, I will aim to answer the six questions above using the information and data published by SART. I will also note when there are limitations to this resource and suggest other resources to explore.
What is IVF?

At its core, in vitro fertilization is the process of stimulating the ovaries to produce multiple eggs, fertilizing those eggs outside of the body, and transferring an embryo back into the uterus to, hopefully, develop into a baby.
However, while these are the key steps in all IVF cycles, the details of each step can vary considerably depending on your specific treatment plan and needs as a patient. Therefore, I prefer to think of IVF as a set of tools - medications, procedures, and lab techniques - that doctors have to help couples conceive rather than as a single treatment or procedure.
SART’s webpage, "A Patient's Guide to ART," is a robust resource for learning more about the IVF process.
In addition, Dr. Aaron Styer provided an excellent overview of IVF in the last issue of this magazine.
Finally, the “What is IVF?” video in my “Considering IVF? Consider This…” series also explains each step in a typical IVF cycle and provides information both about the medical science of IVF and the experience of going through a cycle as a patient.
If you’re preparing to start IVF or are curious to learn more about it, I highly recommend checking out these resources.
Does IVF work?

While this seems like a very reasonable question to ask about any medical procedure, it is often quite hard to answer. Thankfully, we can look at the data published by SART on the birth outcomes of its member clinics as a place to start.
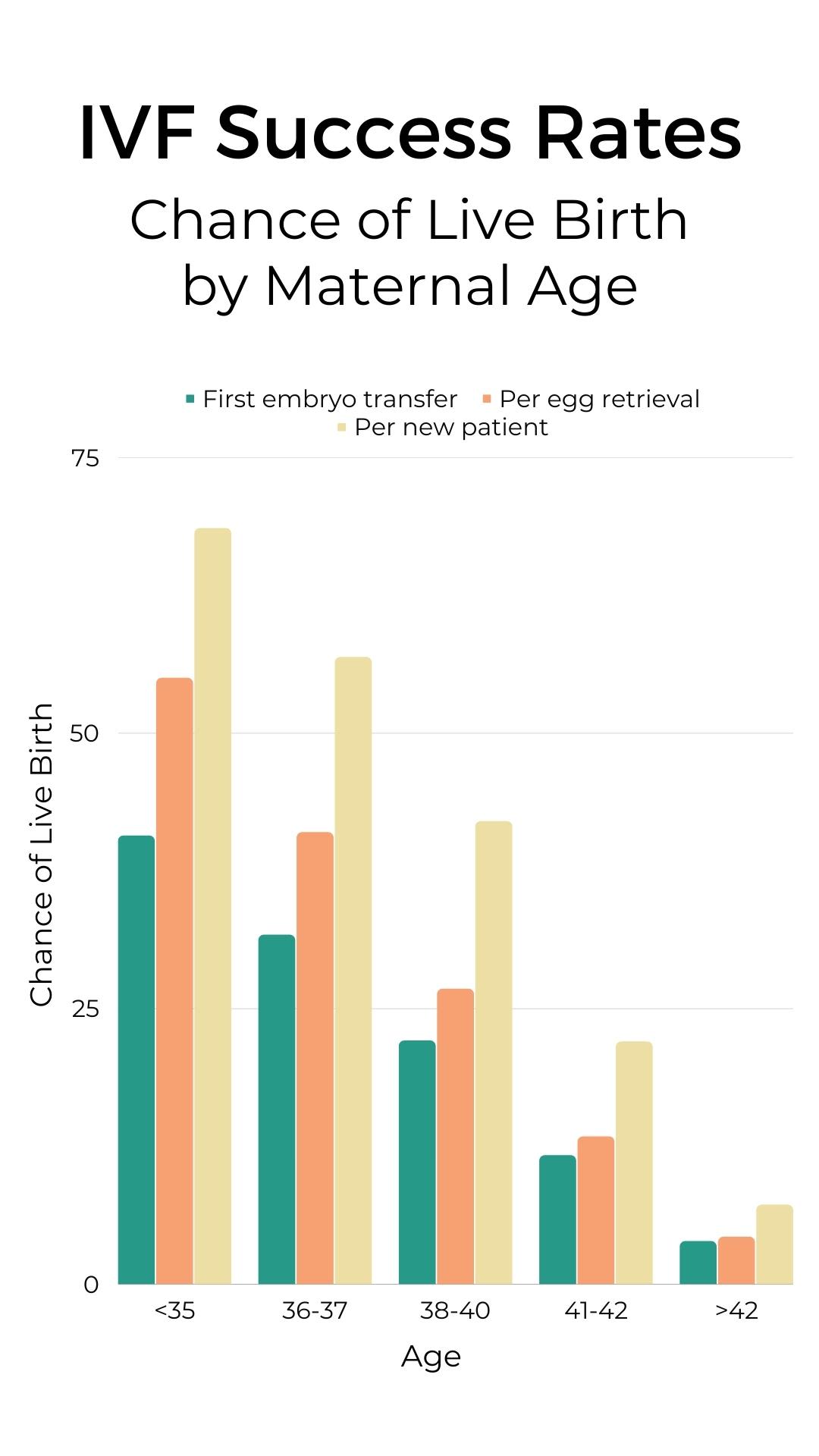
I created this graph from SART’s 2019 annual report. (2019 is the most recent year for which there is complete data).
The graph shows the average live birth rate for all IVF cycles started in 2019, broken down by maternal age. (These numbers exclude donor egg cycles and include all live births, whether singleton, twins, or higher order multiples.)
The teal bars show the average live birth rate for all first embryo transfers. That is, the first embryo(s) transferred following an egg retrieval.
The orange bars show the live birth rate for all complete IVF cycles. That is, the live birth rate resulting from one egg retrieval considering all embryos transferred from that retrieval cycle.
Finally, the yellow bars show the live birth rate for all patients starting IVF in 2019, regardless of the number of IVF cycles or embryo transfers it took to achieve the birth.
So, does IVF work?
The numbers indicate that yes, it does eventually work for some people and that age strongly affects one’s likelihood of success.
Many of us assume that IVF, and medical procedures in general, always work. That doing IVF equals having a baby. So, the numbers presented in this way can come as a shock.
While it is important to have realistic expectations for our medical care, it is also important to note that this data has some limitations.
First, the data only show the IVF outcomes for individual patients at the clinic they started their care at in 2019. However, patients do switch clinics during the course of their care. They might move to a new city, switch insurance carriers and need to find a new in-network doctor, or choose to transfer their care elsewhere for other reasons. As a result, the success rates per patient (yellow bars) may be slightly higher than shown here.
In addition, the data presented in this way assumes a drop out rate of zero. That is, it assumes that patients continue doing IVF until they have a baby. But, we know that this is often not the case. Patients drop out of care for a variety of reasons. Some may only be able to afford one or two IVF cycles. Others may decide that the experience is not for them and choose other means to build their family. Again, this means that the success rate per patient (yellow bars) may be higher than represented here.
Finally, it is important to remember that these numbers are averages. This data clearly shows that IVF success is strongly affected by age. But, there are other individual characteristics that also influence IVF outcomes.
Will IVF work
for me?

The graph above shows that maternal age significantly impacts one's likelihood of success with IVF. But, there are many other things that affect IVF outcomes as well.
For example, Law et al. shows that the number of eggs retrieved in a single cycle is also a strong predictor of success. While younger women are more likely to produce more eggs per stimulation cycle than older women, there remains considerable variation within each age range.
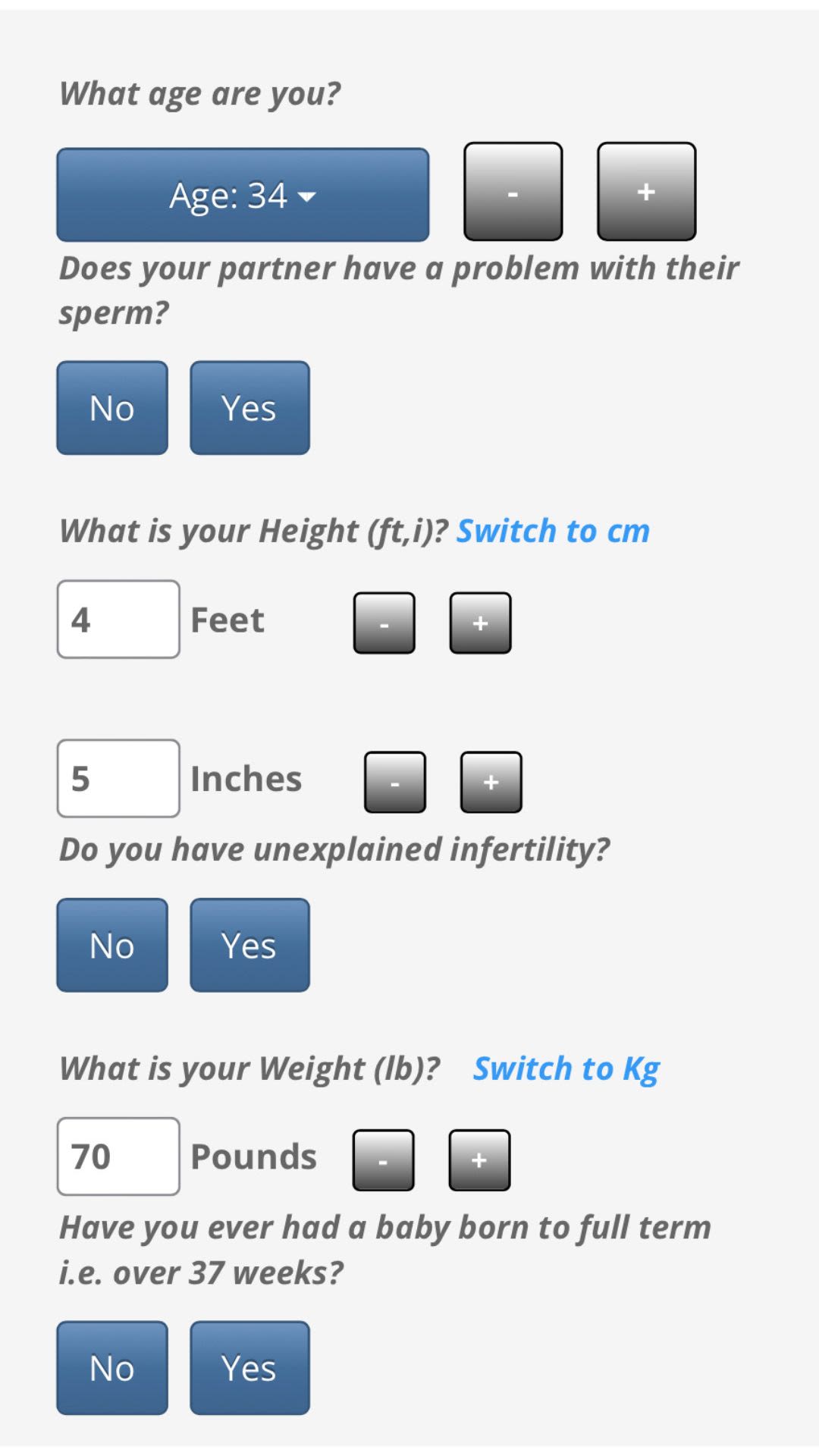
SART’s “Predict My Success” tool attempts to address this. This tool asks a few basic questions like your age, height and weight, and known medical conditions and then estimates your chance of success per egg retrieval (aka your chance of having a baby considering all embryo transfers resulting from a single egg retrieval).
But, as with any health predictor tool, this one isn’t perfect.
It is important to remember that a “personalized prediction” is just the average outcome of people with similar characteristics asked about by the tool.
See SART's tool in action below!
What are the
risks of IVF?

Historically, one of the biggest risks associated with IVF was preterm birth due to twin or high order pregnancies.
Thankfully, due to a combination of technological advances in the field and the work of SART and others to shift standards of care, the chance of twin or higher order pregnancies from IVF has greatly reduced.
According to the SART 2019 data, more than 90% of IVF pregnancies were singleton pregnancies, and between 80% and 90% were delivered at term (after at least 37 weeks). This is similar to the rate of prematurity that is seen in the population as a whole.
However, the SART annual reports do not include data on other risks of treatment.
We know that one of the most serious, immediate risks of IVF is Ovarian Hyperstimulation Syndrome (OHSS). Thankfully, severe or dangerous OHSS occurs in less than 2% of cycles. You can learn more about OHSS here and in the video below.
What does it cost?

Here again, there are many variables that impact the cost of IVF and patients have limited ability to predict what they will pay in advance.
In the US, the average cost of an IVF cycle can range from $12,000 to $17,000 depending on where you live, and this does not include the cost of medications or “add-ons'' such as preimplantation genetic testing (PGT).
Insurance coverage also varies widely, including some states mandating coverage and others leaving the decision to private insurance companies and employers.
While the SART data does not directly address the cost of treatment, it does provide helpful information when budgeting for your care. Looking at the "IVF Success Rates" graph, it is pretty clear that, particularly if you are over the age of 35, most couples would be wise to budget for at least two full cycles of IVF.
Who's the best
doctor for me?

Like the previous question, the data published by SART can not fully answer this question. But, it can serve as a helpful guide.
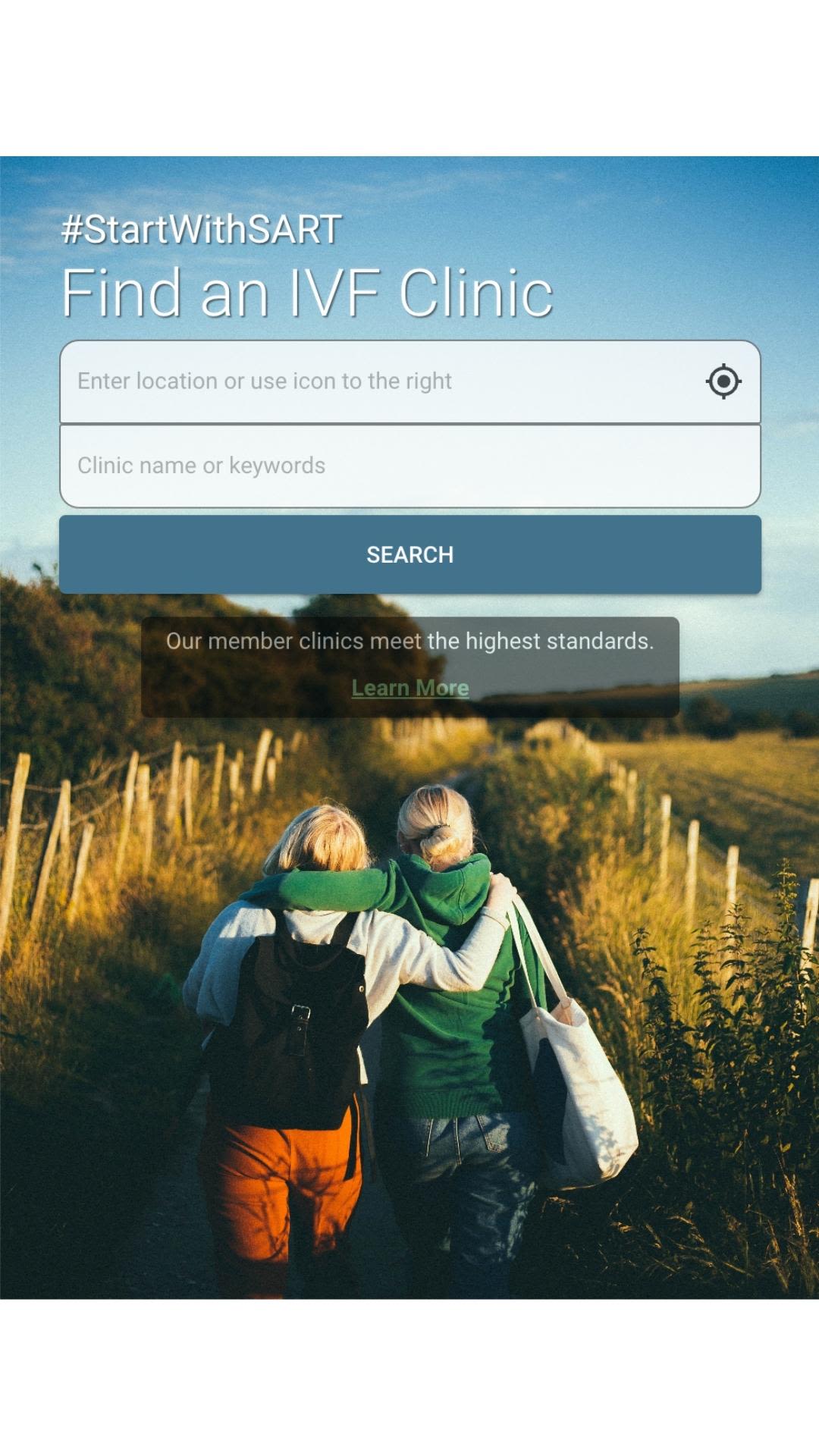
Remember that clinics that are members of SART are held to their high practice standards. Therefore, when considering a doctor at a particular clinic, first check to see that the clinic is a member of SART. You can do this using SART’s “Find A Clinic” tool.
If the clinic you are interested in is a member of SART, you will be able to click on that clinic’s outcomes report. This is structured similarly to the annual reports I mentioned earlier but represents only IVF cycles done at that clinic.
An important thing to understand about these reports is that they are not risk-adjusted. That means that differences in the kinds of patients a clinic treats (e.g. more young patients vs older patients or patients with more complex health issues) are not accounted for. So, if you are comparing clinics and notice small differences in their outcomes, it doesn’t mean that one clinic is better than the other. As a result, I advise my clients not to make too much of those individual clinic reports.
The main thing to look at is the total number of cycles the clinic did in the last year. For any kind of medical procedure, the more you do of it, the better you are at it. So, as a general rule of thumb, you want to see that the clinic is doing at least 100 cycles per doctor per year. But, again, these are rough numbers. A clinic that is doing 80 cycles per doctor per year may be just as good or even better than one doing 120 cycles per doctor per year.
But, one of the most important and overlooked parts of this question is the “for me”.
Two doctors may be equally proficient in their work, but one may make you feel more comfortable than the other. This is important. It can impact every aspect of your experience with your care.
That’s why I always recommend, when possible, setting up initial appointments with a couple of different doctors at different clinics. If one doctor or one clinic just feels more comfortable to you, that’s something important to consider.
In summary, the fertility community is blessed to have SART as a trusted resource.
While the data they publish can’t completely answer all of our questions about IVF, it can be a great place to start.
With help, information and resources, you will hopefully feel more empowered in your family building experience.
Dr. Stephanie Wissig is a non-practicing physician with a mission to improve patient outcomes and experience.
She is an alumna of Barnard College, earned her MD, PhD from Albert Einstein College of Medicine, and has spent much of the last eight years working in the field of Health Outcomes Measurement.
Stephanie is also a Board Certified Patient Advocate, Certified Professional Coach, and Owner/Director of Stephanie Wissig Fertility Support, through which she offers advocacy and coaching to individuals and couples struggling with infertility.
Finally, she is a proud IVF mom.