Unlocking New Answers About Male Fertility
Capacitation - From Discovery to Diagnostic Tool

Imbalance in the Fertility Testing To-Do List
Everyone who struggles to build their family has a different story, but some elements of the journey are familiar to many.
One of those common experiences is navigating that first set of fertility tests.
As a female patient, I left my first reproductive endocrinology appointment with my head spinning. Suddenly my calendar was filled with reminders to schedule “Day Three Labs” and transvaginal ultrasounds. I soon learned the discomfort of an office hysteroscopy. I dutifully arrived for my hysterosalpingogram to assess the shape of my uterus and identify any obstructions in my fallopian tubes or uterine cavity. And while I didn't need laparoscopic surgery to evaluate endometriosis, I know plenty of other women who have.
My husband, on the other hand?
He, like nearly every male partner in the last several decades, only had to undergo a single test to assess his fertility: a semen analysis.
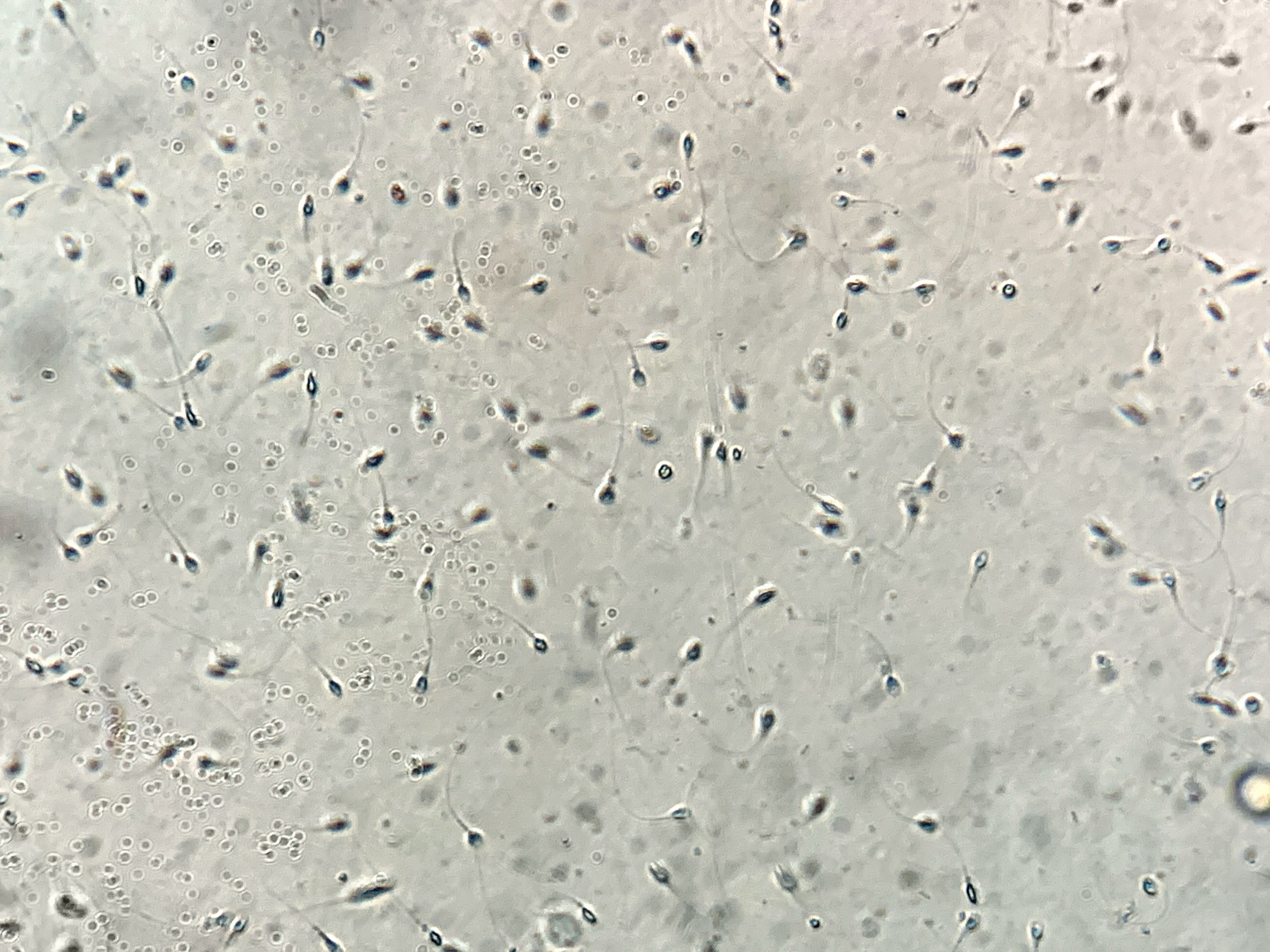
Even though 30% of infertility can be attributed to male factors, as many as half of male infertility cases go undiagnosed by traditional methods. A semen analysis measures sperm count, sperm motility (quality of movement), and sperm morphology (shape, size, and appearance). But what it doesn’t measure is something called capacitation, a necessary biological change that happens directly before fertilization can occur.

What is Capacitation and Why Does it Matter
Capacitation may be the most important fertility term that you've never heard.
During capacitation, changes occur in specific proteins and lipids in the outer layer of a sperm cell to allow it to navigate the complicated cell-matrix surrounding the egg and successfully fertilize it.
Here’s the important part—no matter how well a sperm swims or how perfect its shape, if it cannot capacitate, it cannot fertilize an egg.
Dr. Alexander Travis has spent the last twenty-five years of his career studying capacitation, and his work has led to a new development in male fertility screening: Cap-Score.
How Basic Discovery Science Led to Valuable New Insights
Travis first became interested in capacitation during his doctoral studies at the University of Pennsylvania.
After studying veterinary medicine at Penn, he went on to earn his PhD at Penn’s Center for Research on Reproduction & Women’s Health. Throughout it all, he was curious to learn more about how assisted reproduction could impact wildlife conservation efforts and human fertility challenges.
As a post-doc, he and his fellow researchers made an exciting discovery. When they incubated a sample of sperm with stimuli for capacitation, they saw that a specific lipid (identified as GM1) moved in some sperm but not others. Travis realized that this could be a marker to tell which sperm were capable of fertilization and which were not.
When he moved to Cornell University, Travis conducted numerous follow-up studies to prove that capacitation was indeed predictive of fertility. From there, his lab developed a technique to quantify the number of capacitated sperm in a sample, offering a brand new measure of sperm function.
His colleague Dr. Gianpiero Palermo, one of the inventors of Intracytoplasmic Sperm Injection (ICSI), did the first clinical trial of Cap-Score on real patients at The Ronald O. Perelman and Claudia Cohen Center for Reproductive Medicine of Weill Cornell Medical College.
"We saw a clear correlation," recalls Travis. "Some patients involved in the trial would come in with not just five failed intrauterine insemination (IUI) cycles, but sometimes as many as ten or fifteen from previous clinics. When Dr. Palermo did a Cap-Score, we saw that their history of failure with IUI tracked directly with low Cap-Scores."
At that point, Travis formed biotech company Androvia LifeSciences to turn this laboratory research into a diagnostic tool that could really help people.
The first thing Androvia tackled was gathering a baseline Cap-Score for a fertile population.
They tested men with pregnant partners or young babies, and saw a standard bell curve of scores. They used these findings to establish a cutoff of a Cap-Score around 27.6 as a threshold between normal scores and scores that were low enough to indicate men would struggle to generate a pregnancy.
Next, working with multiple clinics, Androvia gathered data that was reviewed by an independent statistician. It clearly showed a correlation between Cap-Score and successful pregnancy outcomes. In fact, prospective research in 2018 showed that men with normal range Cap-Scores had a four times higher chance of success in their first IUI cycle.
Changing the Approach to Fertility Treatment
At the time of this article’s publication, over 6,000 patient samples have been tested with the Cap-Score.
Dr. Fady Sharara, Medical Director at Virginia Center for Reproductive Medicine and Clinical Professor at George Washington University, was an early adopter. He has since ordered tests for hundreds of his patients to supplement a traditional semen analysis.
“Cap-Score has fundamentality changed the way I approach my work,” Sharara explains. “If you look at just a semen analysis, you only see one view. But when you do a Cap-Score, you suddenly get a panoramic view.”
With the additional insights from Cap-Score, some couples have chosen to move to in vitro fertilization (IVF) faster, knowing that IUI is less likely to succeed based on their score. Having Cap-Score data to make more informed decisions has spared many couples from spending precious time and money - and from heartache. Sharara has even conducted research independent of Androvia that shows patients can improve their Cap-Scores with specific lifestyle changes to achieve better fertility outcomes.
But the thing he cites as the most important benefit is something that, for me as an IVF mom of two, hits close to home.
"The Cap-Score gives men a chance to be an even more involved partner in the journey," Sharara shares. "Fertility struggles can be isolating and overwhelming, and often, women feel like they are the ones responsible for so much. With the knowledge from this test, the male partner may have specific interventions he can take and a deeper understanding of his contribution to the couple's total fertility picture."
The Future of Cap-Score
Though around 60 clinics have ordered Cap-Scores for patients, many doctors are still unfamiliar with this new development in fertility screening. With a low price tag relative to many other fertility expenses, the Cap-Score test could be a game-changer for many couples.
“Since ICSI there has been nothing that has looked at whether a sperm can fertilize and whether a man can improve his sperm’s fertilizing ability,” says Travis.
“The goal of Cap-Score is to give people more information—better information—to help them increase their chances by skipping things that aren’t likely to work and doing things to help them conceive. We really see this as a tool to reduce a lot of stress and heartache, helping more people shorten the path to parenthood.”
So, while Cap-Score’s bench-to-bedside journey took decades, here’s hoping it continues to shorten the fertility journey for many couples in the decades to come.
Amanda Grazioli is a copywriter and brand messaging consultant who helps entrepreneurs and small businesses hone their messages and use the right words to attract more qualified leads and build their brands.
She and her husband are the grateful parents of two daughters, thanks to love, hope, and science.
When she's not writing or engaging in an impromptu dance party with her girls, you can find her experimenting in the kitchen, enjoying nature, and making art. You can learn more about her at amandagrazioli.com.