American Society for Reproductive Medicine Issues New Definition of “Infertility,” More Inclusive of LGBTQ and Single People
The American Society for Reproductive Medicine (ASRM) has updated its definition of “infertility” to make it more inclusive of LGBTQ and single people who seek fertility healthcare. This change could motivate policymakers and insurers to be more inclusive as well, said two experts who spoke with me.

The Need
People may need fertility healthcare for a number of reasons, including problems with their reproductive systems, not having a partner, or not having one with the opposite gamete (egg or sperm). Many insurers, however, only cover such treatment after a medical diagnosis of infertility.
This can mean a requirement to “try naturally” for months before being eligible for treatment (obviously not an option for single people and same-sex couples), or for same-sex couples to pay out of pocket for documented attempts at assisted insemination, while different-sex couples can simply state that they’ve been trying.

Some companies have changed their policies (or, as in a recent case brought by a queer mom against Aetna, been forced to by lawsuit) to cover infertility without such a requirement; many others have not.
Only 21 states plus D.C. have laws mandating any kind of fertility coverage, with only Maine, Illinois, Colorado, and D.C. using definitions clearly and fully inclusive of LGBTQ and single people.


The New Definition

The ASRM’s new definition, announced in October at the organization’s annual meeting, explicitly includes those who need donor gametes for any reason, either as an individual or with a partner, and affirms the need for fertility care regardless of sexual orientation or relationship status:
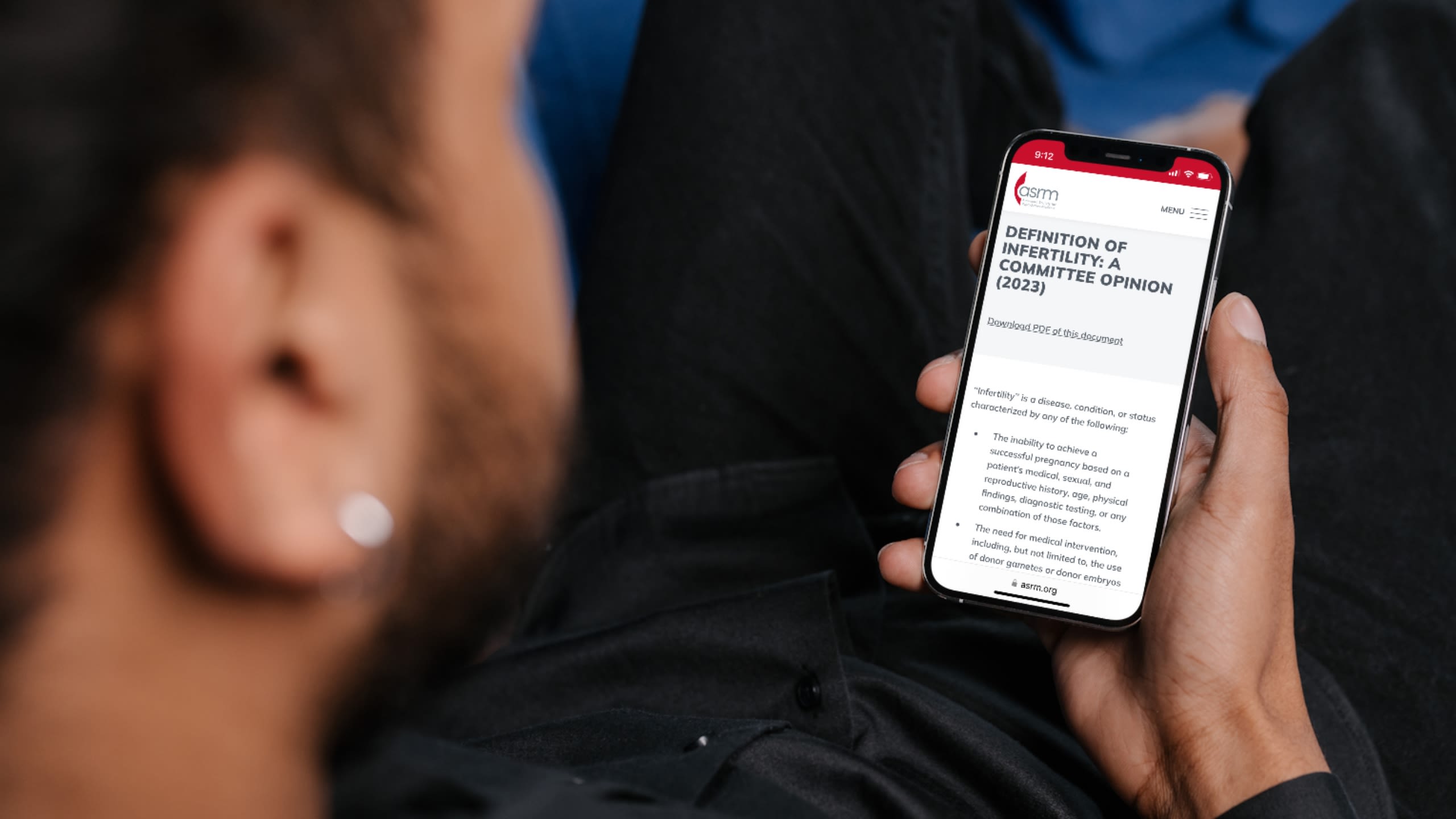
“Infertility” is a disease, condition, or status characterized by any of the following:
• The inability to achieve a successful pregnancy based on a patient’s medical, sexual, and reproductive history, age, physical findings, diagnostic testing, or any combination of those factors.
• The need for medical intervention, including, but not limited to, the use of donor gametes or donor embryos in order to achieve a successful pregnancy either as an individual or with a partner.
• In patients having regular, unprotected intercourse and without any known etiology for either partner suggestive of impaired reproductive ability, evaluation should be initiated at 12 months when the female partner is under 35 years of age and at six months when the female partner is 35 years of age or older.
Nothing in this definition shall be used to deny or delay treatment to any individual, regardless of relationship status or sexual orientation.
ASRM CEO Jared Robins, MD, said in a statement: “This revised definition reflects that all persons, regardless of marital status, sexual orientation, or gender identity, deserve equal access to reproductive medicine. This inclusive definition helps ensure that anyone seeking to build a family has equitable access to infertility treatment and care.”
While the definition in itself carries no legal weight, ASRM guidelines nevertheless have clout. Polly Crozier, director of family advocacy at GLBTQ Legal Advocates & Defenders (GLAD), told me in an interview that she thinks the new definition will be “tremendously influential.” She explained, “Policymakers often cite ASRM guidelines in their definitions…. In the realm of fertility healthcare and what insurance companies will cover, they very much look to ASRM as the standard setters.”
Kate Weldon LeBlanc, executive director of Resolve New England (RNE), an organization dedicated to resources and advocacy for fertility and family building, also told me in an interview that her organization has been pushing for a more inclusive definition of infertility for years. “To have the national reproductive medicine society take that step was really important,” she said. “I think it will be so helpful in many states to highlight that the clinical experts in fertility nationally are taking this more inclusive, broad approach to what infertility is.”
Making a Difference

The new ASRM definition will likely not mean an immediate change to fertility coverage, even in the states that mandate it but have not been inclusive of LGBTQ and single people. “It depends on how the statute is drafted,” Crozier said.
LeBlanc added, “Until a bill passes that changes the definition of infertility that’s in statute, then it’s to some degree up to the discretion of the insurance companies and/or to private employers who provide fertility insurance outside of the mandate.”
The new definition will, however, be “really helpful” to those currently attempting to expand access to fertility care, Crozier said.
“Reproductive justice means the ability to build your family. Many, many, more people than currently have access need access to fertility healthcare.
It’s not just a disease or condition.
In fact, there are many people in our population who need fertility healthcare to build their families because they’re single, because they’re LGBTQ—and that healthcare has to be accessible to a broader swath of people.”
In one example, both GLAD and RNE are part of Fertility Access Connecticut (FACT), a coalition seeking to improve access to fertility care in that state. FACT is pushing for a bill that would require private insurers to cover fertility care for LGBTQ and single people and ensure coverage of fertility care for families insured by HUSKY Health, the state’s public health coverage program. Crozier said she hopes the new ASRM definition will help achieve this, noting, “ASRM is the standard setter for providers in this field, and to have an organization of this magnitude change its definition of what infertility is, I think, will have a tremendously positive impact on policy makers.”
The coalition praised a move this Fall by Connecticut Comptroller Sean Scanlon to extend state employee healthcare coverage so that LGBTQ and single state employees can access fertility healthcare on the same basis as heterosexual, cisgender couples. “Fortunately he had some ability to do it within his own control; he didn’t have to wait for the legislature,” LeBlanc said. “I think all of these things, they’re pieces of the puzzle, and they can make it easier to get the next stage of progress.”
GLAD and RNE are also working on a bill in Vermont, which LeBlanc noted is the only New England state without any fertility insurance law. She said that the new ASRM definition will be helpful because although the bill was already drafted in an inclusive way, the definition “speaks to the fact that that’s the way our field is shifting and that it isn’t just us as an anomaly trying to be inclusive or progressive.”
Room for Improvement

LeBlanc does feel that the new ASRM definition, while a significant step, could be even better. “I would prefer no gendered language at all,” she said. She also wishes it had said “a” female partner instead of “the” female partner, “because it assumes there is a female partner or assumes there’s only one.” Even though there is room for improvement, however, she affirms, “I was so happy to see this.”
Crozier agreed, “It’s not perfect, but I think it goes so much further in really making clear that single people and LGBTQ people should have access to fertility healthcare.”
The Way Forward

In the longer term, the new definition could even help establish fertility coverage under Medicaid, Crozier said, because it frames infertility from the perspective that “many people want to build a family and they should have access to doing that.”
She explained, “We’re really at the beginning of a conversation to say Medicaid programs should cover infertility healthcare. Currently no state in the country has comprehensive fertility healthcare for people who are on Medicaid. I think we need to be considering that it’s not just LGBTQ people or single people on private health insurance, it is everybody in our community who has that desire to build their family.”
LeBlanc also stressed that in addition to the work of organizations in creating change, there is power in individual actions. “The comptroller in Connecticut was motivated by a state employee who brought this inequity to his attention. I think that really speaks to advocacy,” she noted. “It sounds trite, but one person can make a difference.”
The ASRM’s new definition thus gives individuals, organizations, and policymakers a powerful new tool. Crozier said she’s “thrilled” with the news, and asserted, “That core definition of what infertility is drives so much of the conversation on what healthcare is covered by insurance, so it’s really important that definition is right and that it doesn’t exclude people.”


Dana Rudolph is the founder and publisher of Mombian, a two-time GLAAD Media Award-winning blog and resource directory for and about LGBTQ parents, plus a searchable database of 1400+ LGBTQ family books.